When the American Medical Association Speaks, We Listen
I’ve been quite affected by a recent research study published in the Journal of the American Medical Association (JAMA). The research aimed at answering this question: did the Covid-19 pandemic affect the rate of diagnosis of speech delay in children up to the age of five?
The answer was a clear yes. The pandemic did see a great frequency of diagnosis of speech delay in children.
This post is dedicated to acknowledging this reality and proposing solutions to the collateral effect of the pandemic.

Study Key Points:
First, the study was huge. The authors’ analysis covered almost 2.5 million children. They were broken into four groups, one year-olds, two year-olds, three year-olds and four year-olds.
Second, the results were statistically significant. The researchers can be very confident that their findings are not due to chance and are in fact a representation of reality.
Third, they found increased diagnosis across all four age groups analyzed.
Solutions:
Now that we understand this situation is real and the pandemic is the likely cause of a greater prevalence of speech delay, let’s talk about what we can do to address it.
When a parent, teacher or pediatrician first raises a concern about a child’s speech development, the first step is always an evaluation with a licensed speech-language pathologist. Should the evaluation yield a diagnosis of speech delay, the next urgent step is to begin a course of therapy.
For decades, we’ve known of the existence of critical periods of speech development. The periods that children are expected to acquire given skills by a certain age. If a child misses these critical windows of development, rest assured speech therapy has been proven to catch children up. However, the sooner a child can be seen, the better the child’s prognosis.
Once a decision is made to get an evaluation, the next question to answer is where will we get these services? Luckily, there are many ways to do this but they all require a different procedure and have their strengths and drawbacks.
Options to explore:
See below for a list of these options which may be dependent on age, income or employment requirements:
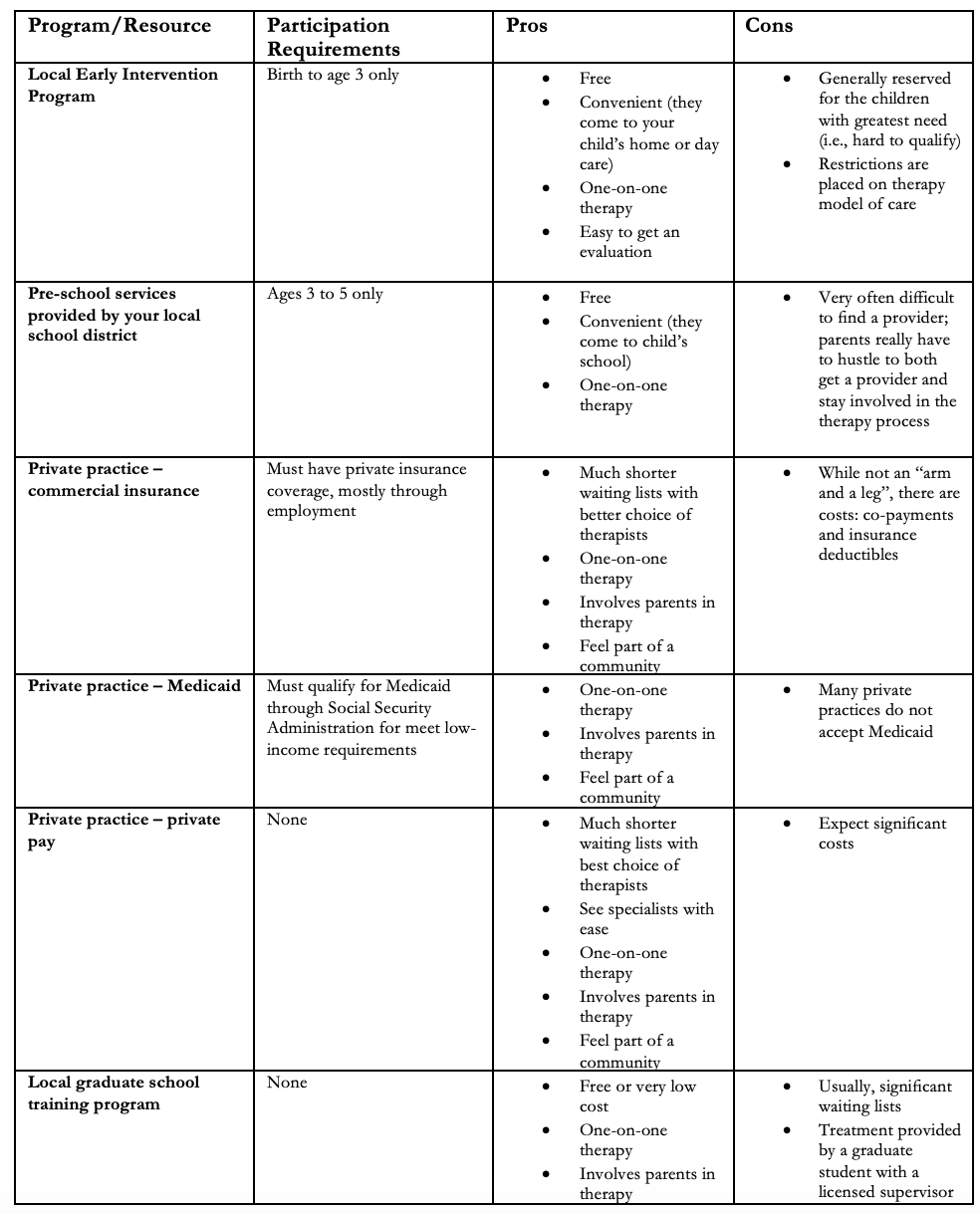
This list is not absolutely exhaustive and other options that may be available to you. Here are a few examples:
Grant funding
TriCare (military insurance)
Therapeutic day schools – more significant developmental or medical needs
Connect:
At Speech Buddies we are committed to providing superior speech therapy solutions for all involved in the process (children, parents, caregivers, educators and fellow therapists).
Our Speech Buddies Tools have strong data to support their use with a wide range of speech delays. We also offer a free online directory for speech therapists nationwide on Speech Buddies Connect.
Lastly, we know the importance of setting up speech therapy promptly following a speech delay diagnosis. Please feel free to email us at info@speechbuddies.com for guidance on how to get started. We’d welcome the opportunity to point you in the right direction of either local, regional or national resources that you’d have available to you.
By Gordy Rogers, M.S. CCC-SLP

Time-Series Analysis of First-Time Pediatric Speech Delays From 2018 to 2022
December 4, 2023 Brianna M. Goodwin Cartwright, MS1; Peter D. Smits, PhD1; Sarah Stewart, MD1; et al Patricia J. Rodriguez, PhD, MPH1; Samuel Gratzl, PhD1; Charlotte Baker, DrPH, MPH, CPH1; Nicholas Stucky, MD, PhD1
JAMA Pediatr. 2024;178(2):193-195. doi:10.1001/jamapediatrics.2023.5226





 meticulous records she kept of Thomas’s condition, Jewett says that her son suffered from five incidents of acute otitis media — the common ear infection — in less than one calendar year.
meticulous records she kept of Thomas’s condition, Jewett says that her son suffered from five incidents of acute otitis media — the common ear infection — in less than one calendar year.